Date 11 Feb 2026
Hair fall and hair loss are often used interchangeably in everyday conversation, but medically they are two very different biological processes. Failing to distinguish between them delays diagnosis, masks early pathology, and reduces the effectiveness of treatment.
In India, hair complaints are rarely caused by a single factor. Genetics, nutrition, endocrine health, pollution, water quality, and psychological stress frequently coexist, creating a complex background where temporary shedding can quietly transition into permanent follicular damage.
Understanding hair fall vs hair loss is required to decide whether reassurance and correction of triggers is sufficient, or whether long-term medical intervention is required to prevent irreversible density loss.
To understand the difference, it is important to first understand how hair normally grows. Every scalp follicle cycles through growth (anagen), regression (catagen), and rest (telogen). At any given time, a portion of hair is expected to shed.
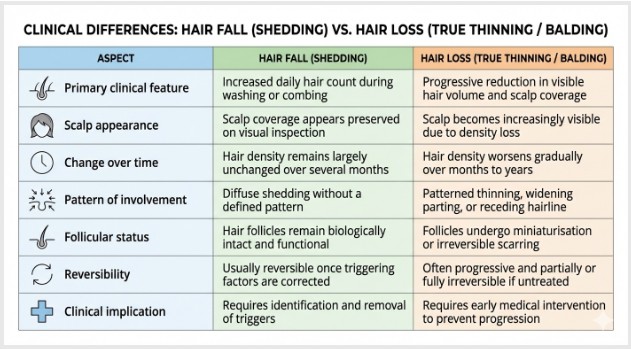
Hair fall refers to excessive shedding without structural follicle damage. The follicles remain capable of producing normal hair once the triggering factor resolves. Hair loss, by contrast, involves progressive follicular miniaturisation or destruction, leading to reduced density over time.
This distinction explains why some individuals experience dramatic shedding yet recover fully, while others lose hair gradually without noticing heavy fall, until visible thinning becomes undeniable.
|
Aspect
|
Hair Fall (Shedding)
|
Hair Loss (True Thinning / Balding)
|
|
Primary clinical feature
|
Increased daily hair count during washing or combing
|
Progressive reduction in visible hair volume and scalp coverage
|
|
Scalp appearance
|
Scalp coverage appears preserved on visual inspection
|
Scalp becomes increasingly visible due to density loss
|
|
Change over time
|
Hair density remains largely unchanged over several months
|
Hair density worsens gradually over months to years
|
|
Pattern of involvement
|
Diffuse shedding without a defined pattern
|
Patterned thinning, widening parting, or receding hairline
|
|
Follicular status
|
Hair follicles remain biologically intact and functional
|
Follicles undergo miniaturisation or irreversible scarring
|
|
Reversibility
|
Usually reversible once triggering factors are corrected
|
Often progressive and partially or fully irreversible if untreated
|
|
Clinical implication
|
Requires identification and removal of triggers
|
Requires early medical intervention to prevent progression
|
Misinterpreting early signs of hair loss as “just hair fall” is one of the most common reasons patients present late, when non-surgical options are already limited.
Also Read- Hair Transplant: Understanding the Procedure, Benefits and Risks
Studies consistently show that 50–100 hairs per day fall naturally as part of the telogen phase. Some individuals may shed slightly more without pathology.
The concern begins not with absolute numbers, but with persistence and pattern. When elevated shedding continues beyond six to eight weeks and is accompanied by visible change in scalp appearance, it often signals a shift from reversible shedding to evolving hair loss.
This distinction is critical because telogen effluvium, extremely common due to stress, illness, or nutritional deficiency, can overlap visually with early androgenetic alopecia.
Red flags that suggest shedding is no longer benign:
Persistent daily shedding beyond 150 hairs for several weeks
Reduced ponytail circumference or limp hair texture
Increased scalp visibility under normal lighting
Lack of recovery despite removal of obvious triggers
The key differentiator is failure to regain baseline density after the triggering factor resolves.
Hair loss does not occur suddenly. It progresses through recognisable stages driven by gradual follicular changes. These stages differ between men and women, but the underlying principle, progressive follicle compromise, remains the same.
Recognising these stages early allows intervention while follicles are still salvageable. Ignoring them results in irreversible loss that no topical or injectable therapy can reverse.
Hair loss progression typically follows:
Early, subtle density changes unnoticed in daily grooming
Gradual miniaturisation producing thinner, shorter hair shafts
Loss of terminal hair replaced by fine vellus-like hair
Eventual follicular inactivity or fibrosis
By the time bald patches are obvious, the disease process has often been active for years.
More to Read- The Future of Hair Restoration: Stem Cell Therapy and PRP vs. Traditional Transplants
Male pattern hair loss remains the most common cause of progressive thinning in Indian men. Contrary to popular belief, it is not limited to older age groups and frequently begins in the mid-twenties.
Early changes often appear as mild temple recession or crown thinning, which are easily dismissed as styling issues or stress-related hair fall. This delay allows dihydrotestosterone-mediated miniaturisation to progress unchecked.
As the condition advances, hair shafts become progressively finer, growth cycles shorten, and the scalp becomes increasingly visible. At advanced stages, only the occipital and temporal donor zones remain unaffected.
Once miniaturisation crosses a critical threshold, medical therapy can stabilise but not restore lost density, making detection of early signs of hair loss essential.
Hair loss in women is under-recognised and frequently mislabelled as “hair fall.” This is partly due to preserved frontal hairlines and diffuse thinning patterns that lack obvious bald patches.
In Indian women, androgenetic alopecia often presents as widening of the central parting, reduced overall volume, and increased scalp show under light. Hormonal fluctuations, iron deficiency, and metabolic disorders commonly accelerate this process.
Unlike men, women frequently experience overlapping conditions, such as telogen effluvium masking underlying patterned loss, making diagnosis more complex and treatment delays more common.
Advanced stages can cause profound psychological distress, particularly because hair density plays a central role in cultural and social identity.
Hair thinning rarely results from a single factor. Instead, genetics, lifestyle habits, environmental exposure, and nutritional status often interact, making the distinction between temporary hair fall and progressive hair loss clinically complex.
1.) Genetics and Hormonal Influence
Androgenetic alopecia remains the most common cause of progressive hair loss in India, frequently beginning in men as early as their twenties. The action of dihydrotestosterone (DHT) shortens the hair growth cycle, leading to gradual follicular miniaturisation rather than sudden shedding.
2.) Nutritional Deficiencies
Indian studies consistently associate diffuse hair fall, particularly in women, with iron deficiency, low ferritin levels, vitamin D insufficiency, and inadequate protein intake. Surveys among Indian healthcare professionals also highlight nutritional deficiency as a common cofactor in androgenetic alopecia.
3.) Stress, Lifestyle, and Environmental Factors
Chronic academic or occupational stress can trigger telogen effluvium, causing sudden diffuse shedding months after the stressor. Poor sleep, smoking, alcohol use, hard water, pollution, and aggressive hair practices further weaken hair shafts and scalp health.
4.) Medical Conditions
Systemic disorders such as thyroid disease, PCOS, autoimmune conditions, chronic infections, and post-COVID states are well-documented contributors to hair thinning and loss in Indian adults.
1.) Track Shedding and Visual Changes
Start by paying attention to how much hair you lose on wash days. A few extra strands occasionally are normal, but if you consistently notice well over 100–150 hairs for several weeks, it’s worth taking seriously. Alongside this, take monthly photos of your hairline, crown, and parting under similar lighting. Subtle changes often show up in pictures before they’re obvious in the mirror.
2.) Notice Pattern Shifts in Styling
Changes in how your hair behaves are often early warning signs. Men may notice an “M-shaped” hairline forming, thinning at the crown, or the need to style hair differently to hide scalp. Women often observe a widening centre part, a thinner ponytail, or increased scalp visibility in bright sunlight.
3.) Consider Family History and Age
Genetics play a major role in hair loss. If close family members experienced significant thinning or baldness in their twenties or thirties, your own risk is higher. Indian dermatologists increasingly see androgenetic alopecia in younger adults, challenging the idea that hair loss only happens later in life.
4.) Watch for Associated Scalp or Health Signals
Symptoms like itching, redness, scaling, painful bumps, or sudden patchy hair loss suggest inflammatory, infectious, or autoimmune conditions rather than routine genetic thinning. Similarly, sudden diffuse shedding after illness, surgery, childbirth, or crash dieting often points to telogen effluvium, which is usually reversible but still needs guidance.
Important: If these signs persist for more than three to six months, especially with visible thinning, it’s best to consult a dermatologist or trichologist rather than relying solely on online remedies.
Understanding hair fall vs hair loss separates timely action from delayed regret. Hair fall is often reversible when the underlying hair thinning causes are identified early. Hair loss, especially once it progresses through advanced stages for hair loss, becomes far harder to reverse.
The real challenge is recognising the early signs of hair loss, subtle changes in density, parting, or hairline, before visible baldness appears.
If you are unsure where you stand on the spectrum of hair fall vs hair loss, the most practical next step is expert evaluation. Talk to our with experienced specialists at Eternelle Aesthetics, who will accurately identify your stage, uncover hidden hair thinning causes, and plan evidence-based treatment before irreversible loss sets in.
Losing 50–100 hairs daily is normal if your overall volume stays the same. If heavy shedding continues and you notice thinning, a receding hairline, or widening part, it’s time to see a specialist.
Severe stress can trigger temporary shedding called telogen effluvium. While it often reverses, ongoing stress can worsen genetic hair thinning and accelerate true hair loss if left unaddressed.
Hair oils help reduce dryness and breakage but cannot stop genetic thinning or fix nutritional deficiencies. In real hair loss, they work only as support alongside medical and lifestyle treatment.
Yes, women can develop pattern hair loss. It usually shows as widening of the central part and overall thinning, not bald patches, and is often mistaken for simple hair fall.
Hair transplants are considered when medical treatment has stabilised hair loss but density cannot return naturally. They work best after controlling ongoing thinning, nutrition issues, and scalp health.
